Clinical Trial Finds Diet Works for Depression.
Pioneering new study suggests healthy food can be a powerful antidepressant.
 Pioneering research from the Land Down Under helps you get out from under your depression!
Pioneering research from the Land Down Under helps you get out from under your depression!
Felice Jacka PhD is a trailblazing researcher at Deakin University in Australia who is calling the world’s attention to the powerful impact of food on mood. On January 30, 2017, the journal BMC Medicine published her new randomized controlled study called The SMILES Trial (link is external). This groundbreaking research demonstrates for the first time that people with moderate to severe depression can improve their mood by eating a healthier diet.
You may be surprised to hear that this kind of study has never been done before, probably because you have read headlines in the past proclaiming that healthier diets decrease risk for depression. We have Professor Jacka and her team to thank for many of those hopeful headlines. Over the past seven years, she published numerous epidemiological (survey-based) studies suggesting that people who report eating an unhealthy diet are more likely to be depressed. However, since these studies were based on questionnaires and weren’t actual diet experiments, they didn’t have the power to demonstrate that unhealthy diets could worsen depression symptoms, and couldn’t show that healthy diets could be used to help TREAT depression. These were simply educated guesses that hadn’t been tested in the real world yet. Until now.
Professor Jacka boldly went where no one has gone before: she tested her theories on actual people with clinical depression…and emerged victorious.
The Study
Professor Jacka’s team recruited 67 men and women with moderate to severe depression who reported eating a relatively unhealthy diet. Most were taking antidepressants and/or were in regular psychotherapy.
They put half of these depressed people on a modified Mediterranean diet (aka the “ModiMed” diet—more details below) and required them to attend dietary support sessions with a nutritionist.
The other half continued eating their usual unhealthy diet, but were required to attend social support “befriending” sessions.
Before and after the 12-week study, everyone’s depression symptoms were graded using several different tests. The test this research group chose to focus on was the MADRS scale (Montgomery–Åsberg Depression Rating Scale (link is external)), which rates mood on a scale of 0 to 60, with 60 being the most severely depressed.
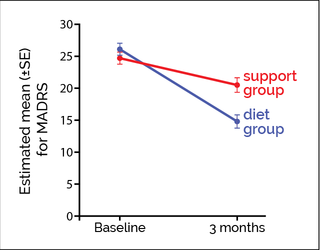
After 12 weeks, people in the ModiMed diet group saw their MADRS scores improve on average by about 11 points. Thirty-two percent (10 out of 31 completers) had MADRS scores so low that they no longer met criteria for depression—remission!
People in the unhealthy diet group improved by only about 4 points on the MADRS test and only 8% (2 of 25 completers) achieved remission.
More happy details:
Calories were not restricted and body weight stayed about the same for everyone in the study, so people didn’t have to lose weight to feel better.
Surprisingly, the ModiMed diet cost about 19% less than the standard unhealthy diet.
The diet plan was apparently easier to stick to than the social support plan, since more people in the diet group (31 out of 33) made it all the way to the end of the study, compared to only 25 out of 34 people in the support group.
What is the ModiMed diet?
 Encouraged foods: whole grains, fruits, vegetables, legumes, low-fat/ unsweetened dairy, raw unsalted nuts, lean red meat, chicken, fish, eggs, and olive oil
Encouraged foods: whole grains, fruits, vegetables, legumes, low-fat/ unsweetened dairy, raw unsalted nuts, lean red meat, chicken, fish, eggs, and olive oil
Discouraged foods: sweets, refined cereals, fried food, fast food, processed meat.
Beverages: maximum two sugar-sweetened beverages per week and maximum two alcoholic drinks per day, preferably red wine.
So, what is so special about the ModiMed diet?
Well, THAT is the $64,000 question, and the answer is? We don’t know.
It could be that this diet was higher in some potentially magical ingredient like olive oil or nuts.
It could be that this diet was lower in some potentially evil ingredient like processed meat or refined carbohydrates.
It could be both.
My opinion, based on everything I know about food and the brain, is that this diet is better than the average diet because:
1. It is extremely low in refined carbohydrates (sugar, flour, refined cereals, etc). These non-foods put your blood sugar, insulin, hormones, and neurotransmitters on a dangerous invisible roller coaster. This destabilizes mood and increases risk for insulin resistance, which causes brain damage over time.
2. It contains plenty of natural fat and cholesterol, which the brain needs to function properly [in my opinion the ModiMed diet unnecessarily limits saturated animal fats].
3. It is low in processed oils from seeds such as cottonseed, safflower and corn. These industrially-refined oils are very high in omega-6 fatty acids (link is external), which tilt the brain towards inflammation and away from healing.
4. It contains animal sources of protein, which are rich in key brain nutrients (link is external) such as iron, zinc, and vitamin B 12. Meat, seafood and poultry are free of anti-nutrients, which interfere with protein and mineral absorption.
5. It is based primarily on whole foods, which humans are well-adapted to eating.
Real Hope for the Real World
I love this study, because it proves that the human brain cares deeply about what we eat. Don’t get me wrong—I prescribe medications every day and I have seen them work wonders. But clearly the most powerful way to fundamentally change your brain chemistry is through food, because that’s where the brain chemicals come from in the first place! I believe a healthy diet can in many cases reduce or eliminate the need for prescription medications.
With the exception of crisis situations and special barriers to dietary change, why not start by improving the quality of your diet? What do you have to lose? Healthy diets have no co-pays, no side effects, and are good for the whole body, not just the brain. I realize that lifestyle changes aren't easy, and they are particularly difficult if you are depressed. For those of my patients who are so depressed that they can't manage trying to change their diet, I recommend starting with medication, therapy, and other interventions first until they start feeling better, and then begin working on their nutrition goals.
For those of you who have tried a Mediterranean diet without success, there is still tremendous hope. There are other healthy changes worth trying—my two favorite recommendations being:
1. Lowering overall carbohydrate intake, especially if you have insulin resistance (link is external).
2. Removing grains and legumes, which interfere with the absorption of key nutrients (link is external) the brain needs to work properly, such as iron and zinc.
For those of you who eat a low-fat, vegan, vegetarian, low-carb, or Paleo diet, this study cannot tell you whether or not the ModiMed diet is better for depression than your diet. I personally eat and advocate for a pre-agricultural whole foods diet (without grains, legumes, dairy, or processed foods) and believe that it should perform even better than the ModiMed diet. However, until we have studies that compare different diets to each other, the only way for you to know which diet works best for your mood is to experiment with them yourself.
Take a Bite Out of Your Depression!
The bottom line is this: the ModiMed diet is clearly superior to a junky standard diet loaded with fast food, processed foods, and refined carbohydrates. It is also affordable and manageable in the real world!
For those of you who don’t care to try the ModiMed diet, there are MOUNDS of evidence incriminating the refined carbohydrates and industrially-produced foods that form the basis of our American diet. So, regardless of what is IN your favorite diet, make sure you get the junk OUT.
Your brain, your metabolism, and your whole body will be happier and healthier.
 Pioneering research from the Land Down Under helps you get out from under your depression!
Pioneering research from the Land Down Under helps you get out from under your depression!Felice Jacka PhD is a trailblazing researcher at Deakin University in Australia who is calling the world’s attention to the powerful impact of food on mood. On January 30, 2017, the journal BMC Medicine published her new randomized controlled study called The SMILES Trial (link is external). This groundbreaking research demonstrates for the first time that people with moderate to severe depression can improve their mood by eating a healthier diet.
You may be surprised to hear that this kind of study has never been done before, probably because you have read headlines in the past proclaiming that healthier diets decrease risk for depression. We have Professor Jacka and her team to thank for many of those hopeful headlines. Over the past seven years, she published numerous epidemiological (survey-based) studies suggesting that people who report eating an unhealthy diet are more likely to be depressed. However, since these studies were based on questionnaires and weren’t actual diet experiments, they didn’t have the power to demonstrate that unhealthy diets could worsen depression symptoms, and couldn’t show that healthy diets could be used to help TREAT depression. These were simply educated guesses that hadn’t been tested in the real world yet. Until now.
Professor Jacka boldly went where no one has gone before: she tested her theories on actual people with clinical depression…and emerged victorious.
The Study
Professor Jacka’s team recruited 67 men and women with moderate to severe depression who reported eating a relatively unhealthy diet. Most were taking antidepressants and/or were in regular psychotherapy.
They put half of these depressed people on a modified Mediterranean diet (aka the “ModiMed” diet—more details below) and required them to attend dietary support sessions with a nutritionist.
The other half continued eating their usual unhealthy diet, but were required to attend social support “befriending” sessions.
Before and after the 12-week study, everyone’s depression symptoms were graded using several different tests. The test this research group chose to focus on was the MADRS scale (Montgomery–Åsberg Depression Rating Scale (link is external)), which rates mood on a scale of 0 to 60, with 60 being the most severely depressed.
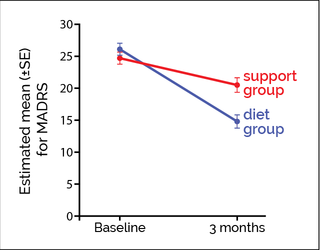
After 12 weeks, people in the ModiMed diet group saw their MADRS scores improve on average by about 11 points. Thirty-two percent (10 out of 31 completers) had MADRS scores so low that they no longer met criteria for depression—remission!
People in the unhealthy diet group improved by only about 4 points on the MADRS test and only 8% (2 of 25 completers) achieved remission.
More happy details:
Calories were not restricted and body weight stayed about the same for everyone in the study, so people didn’t have to lose weight to feel better.
Surprisingly, the ModiMed diet cost about 19% less than the standard unhealthy diet.
The diet plan was apparently easier to stick to than the social support plan, since more people in the diet group (31 out of 33) made it all the way to the end of the study, compared to only 25 out of 34 people in the support group.
What is the ModiMed diet?
 Encouraged foods: whole grains, fruits, vegetables, legumes, low-fat/ unsweetened dairy, raw unsalted nuts, lean red meat, chicken, fish, eggs, and olive oil
Encouraged foods: whole grains, fruits, vegetables, legumes, low-fat/ unsweetened dairy, raw unsalted nuts, lean red meat, chicken, fish, eggs, and olive oilDiscouraged foods: sweets, refined cereals, fried food, fast food, processed meat.
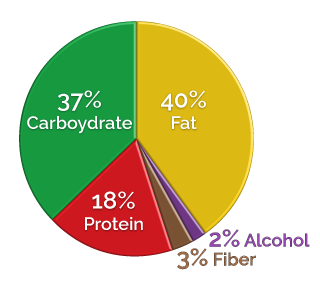
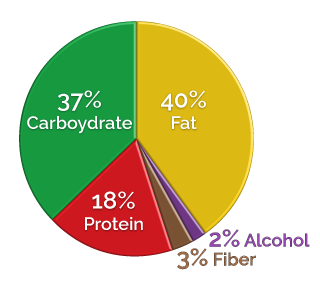
Beverages: maximum two sugar-sweetened beverages per week and maximum two alcoholic drinks per day, preferably red wine.
So, what is so special about the ModiMed diet?
Well, THAT is the $64,000 question, and the answer is? We don’t know.
It could be that this diet was higher in some potentially magical ingredient like olive oil or nuts.
It could be that this diet was lower in some potentially evil ingredient like processed meat or refined carbohydrates.
It could be both.
My opinion, based on everything I know about food and the brain, is that this diet is better than the average diet because:
1. It is extremely low in refined carbohydrates (sugar, flour, refined cereals, etc). These non-foods put your blood sugar, insulin, hormones, and neurotransmitters on a dangerous invisible roller coaster. This destabilizes mood and increases risk for insulin resistance, which causes brain damage over time.
2. It contains plenty of natural fat and cholesterol, which the brain needs to function properly [in my opinion the ModiMed diet unnecessarily limits saturated animal fats].
3. It is low in processed oils from seeds such as cottonseed, safflower and corn. These industrially-refined oils are very high in omega-6 fatty acids (link is external), which tilt the brain towards inflammation and away from healing.
4. It contains animal sources of protein, which are rich in key brain nutrients (link is external) such as iron, zinc, and vitamin B 12. Meat, seafood and poultry are free of anti-nutrients, which interfere with protein and mineral absorption.
5. It is based primarily on whole foods, which humans are well-adapted to eating.
Real Hope for the Real World
I love this study, because it proves that the human brain cares deeply about what we eat. Don’t get me wrong—I prescribe medications every day and I have seen them work wonders. But clearly the most powerful way to fundamentally change your brain chemistry is through food, because that’s where the brain chemicals come from in the first place! I believe a healthy diet can in many cases reduce or eliminate the need for prescription medications.
With the exception of crisis situations and special barriers to dietary change, why not start by improving the quality of your diet? What do you have to lose? Healthy diets have no co-pays, no side effects, and are good for the whole body, not just the brain. I realize that lifestyle changes aren't easy, and they are particularly difficult if you are depressed. For those of my patients who are so depressed that they can't manage trying to change their diet, I recommend starting with medication, therapy, and other interventions first until they start feeling better, and then begin working on their nutrition goals.
For those of you who have tried a Mediterranean diet without success, there is still tremendous hope. There are other healthy changes worth trying—my two favorite recommendations being:
1. Lowering overall carbohydrate intake, especially if you have insulin resistance (link is external).
2. Removing grains and legumes, which interfere with the absorption of key nutrients (link is external) the brain needs to work properly, such as iron and zinc.
For those of you who eat a low-fat, vegan, vegetarian, low-carb, or Paleo diet, this study cannot tell you whether or not the ModiMed diet is better for depression than your diet. I personally eat and advocate for a pre-agricultural whole foods diet (without grains, legumes, dairy, or processed foods) and believe that it should perform even better than the ModiMed diet. However, until we have studies that compare different diets to each other, the only way for you to know which diet works best for your mood is to experiment with them yourself.
Take a Bite Out of Your Depression!
The bottom line is this: the ModiMed diet is clearly superior to a junky standard diet loaded with fast food, processed foods, and refined carbohydrates. It is also affordable and manageable in the real world!
For those of you who don’t care to try the ModiMed diet, there are MOUNDS of evidence incriminating the refined carbohydrates and industrially-produced foods that form the basis of our American diet. So, regardless of what is IN your favorite diet, make sure you get the junk OUT.
Your brain, your metabolism, and your whole body will be happier and healthier.


Comments
Post a Comment